To the knowledge of scientists and the CDC, the family of coronaviruses has been around since the mid-1960s. One of the most deadly of these viruses came about in the early 2000s when Severe Acute Respiratory Syndrome, otherwise known as SARS, emerged in China. A decade later, the Middle East Respiratory Syndrome (MERS) developed in Saudi Arabia, spawning another outbreak.
SARS-CoV-2 — what we now refer to as COVID-19 — is one of the top-three most severe of seven coronaviruses that humans have contracted over the last 20 years. The Novel Coronavirus is particularly notable in its ability to transmit itself at an alarming rate and to mutate rapidly along the way. The WHO has determined that the average carrier of the virus will transmit it to at least two or three others before ever even showing symptoms, making this the most contagious and concerning outbreak since the influenza pandemic over a century ago.
As Novel Coronavirus works its way through the population, researchers are hot on its heels determining what makes this virus so successful in transmission, how it’s evolving, and what this means for the population. Here, we will discuss our findings on how the genetic sequence of COVID-19 is able to mutate so quickly over a short period of time and the implications of this phenomenon for the world.
The Origins of Novel Coronavirus
Late in December of 2019, the WHO discovered that a new coronavirus strain had arisen in Wuhan, China, and named it SARS-CoV-2. While the origins of this strain are still heavily debated, research has confirmed that the virus was naturally hosted and evolutionarily shaped by bats.
The real cause for concern is that this virus can remain stable on surfaces for hours, including cardboard for 24 hours, copper for four hours, and up to three days on plastic and stainless steel. Those who have unknowingly contracted COVID-19 can be asymptomatic for at least two weeks, after which they may develop symptoms of fatigue, a fever, a dry cough, and/or difficulty breathing. As of March 26, 2020, there were nearly half a million infected across the globe and over 20,000 reported dead — most of whom were older, with preexisting medical conditions.
Method of COVID-19 Transmission
COVID-19 spreads much faster than the original SARS, infecting more than ten times the number of people. This respiratory condition spreads through droplets of an infected person’s coughing, sneezing, or discharge from the nose.
The current theory is that the Novel Coronavirus has a special “spike” protein that binds to a cell membrane via an enzymatic activation. Scientists have learned through genomic analysis that the spike protein has a site activated by human and animal host cell enzymes called furin, which is found in a wide variety of human tissues. So potentially, the virus may be able to attack multiple organs simultaneously, according to a structural biologist at Huazhong University of Science and Technology in Wuhan. The activation site seems to allow easier entry into cells for this particular strain and could potentially influence the stability and transmission rate of the virus, based on the research of a Cornell University virologist.
COVID-19 Transmissions

Debunking the Popular Coronavirus Myth
Considering the devastating impact COVID-19 has had on the world so quickly, it’s tempting to believe the myth that this virus was intentionally manufactured in a lab. A research team at the Scripps Research Institute has proved otherwise; their genetic analysis of the Novel Coronavirus origins and comparison to available genome sequence data for other known strains of coronavirus proved that this new strain originated through natural processes and has a 96.2% similarity to a bat SARS-related coronavirus.
Further evidence of COVID-19’s natural origins is that the structure of the SARS-CoV-2 molecular backbone does not resemble that of a virus known to cause illness, which would have been the case if it were purposefully engineered to be a dangerous pathogen. Instead, its backbone more closely resembles natural and common viruses found in pangolins and bats.
Sequencing the SARS-CoV-2 Genome to Identify Distinct Features
As soon as the epidemic in China began, the nation’s scientists began sequencing the genome of this strain and made their results publicly available to researchers across the globe so they could contribute to the further understanding of this virus. The data that resulted from their work highlighted the ease of human-to-human transmission and gave them insight that this would turn into an epidemic. Scripps and other researchers including us at Psomagen have since been using sequencing data to determine the evolution of the virus by focusing on uniquely distinct features.
In their research so far, scientists in China have successfully sequenced the entire genome of at least 115 samples of the virus. The data strongly suggests that it was initially hosted by an animal before transmitting itself to humans. Bats are the most strongly suspected origin hosts because there is minimal difference between the RNA samples of a bat virus taken in Wuham and the samples from those hospitalized early in the outbreak.
According to research findings on the COVID-19 genome, the virus mutates 24 times each year or twice per month, which is similar to the mutation rate of the flu. However, Novel Coronavirus has a longer genome than the flu, meaning there are fewer mutations per base. This is normal and to be expected, as viral mutations are a natural part of the lifecycle of a virus. But what does this mean? Well, science says these mutations mean that we’re all experiencing a slightly different coronavirus from country to country.
Diversity of COVID-19

How Is the Coronavirus Strain Evolving From Country to Country?
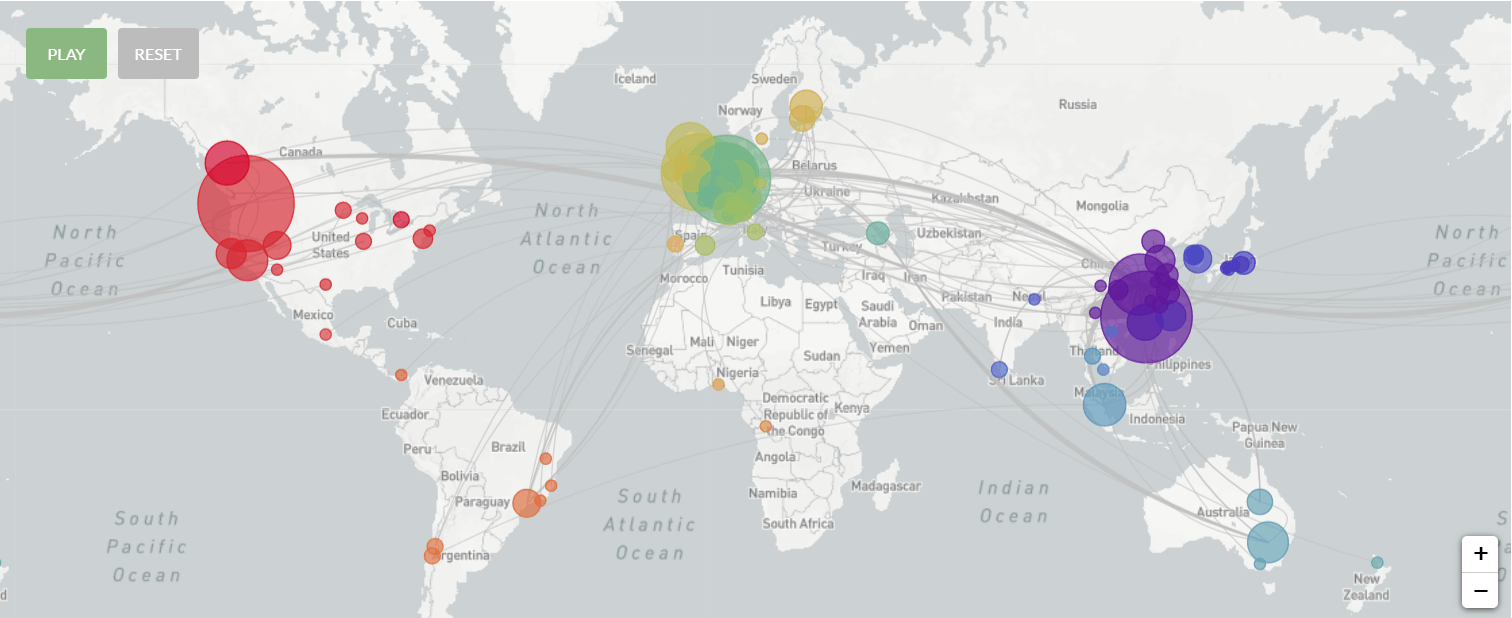
We now know from all of the compiled research that there have been a number of different versions of the Novel Coronavirus throughout the course of this pandemic. But how does this happen? Think of the small genetic code changes in the virus as fingerprints used by geneticists to track its movements around the globe in real time. Viruses are best able to evolve as they transmit from one person to another — it’s kind of like the telephone game. Mistakes are made as the message is passed down the line of participants.
In a virus’ genetic code, the mistakes can be very small and simple changes like an adenosine changing to a thymine or a guanine to a cytosine. While these genetic code alterations can’t do much on their own to change the way the virus behaves, geneticists can collect a large number of samples and construct a tree of viral descent. Comparing the genetic code of each person’s infection and tracing them back to their sources can reveal how the virus reached its present state, how transmission occurred, and whether the mutations made the virus more deadly.
This is precisely how Chinese researchers were able to determine how COVID-19 jumped from bats to people, and this information has helped science to say definitively that the month of December, 2019, was when the strain emerged in humans.
685 Genomes

Implications for the Present and the Future
Cases of COVID-19 are cropping up rapidly, and it’s difficult to say what the future looks like. However, we’re fortunate to have a good amount of information about the evolution of COVID-19 and a decent pool of data showing how to quickly interrupt the transmission. Hand washing and social distancing are the most basic measures of reducing transmission and slowing the pandemic — but only when a significant portion of the population follows that protocol.
This means that, until we can contain and mitigate the spread, every individual must do their part to stay home as much as possible, wash their hands thoroughly, avoid touching their face, and stay at least six feet away from other individuals when they must venture out. As we do so, this virus will be stopped in its tracks. Importantly, we will also gain a better understanding of how to handle the next pandemic when it inevitably occurs.